Health Stories
Eye care centre welcomes Lebanese ophthalmologist
Eye care centre welcomes Lebanese ophthalmologist

MHC’s Eye Care Centre of Excellence is proud to welcome Dr. Charbel Wahab who recently started a one-year fellowship with the Retina Fellowship Program.
Dr. Wahab, who was born and raised in Lebanon, moved to Winnipeg from Toronto where he completed his medical retina fellowship at the University of Toronto.
He said he decided to look into the surgical retina program in Winnipeg after hearing really great feedback about MHC.
“I had a colleague in Toronto who told me about the surgical department here and the high load of patients needing surgery,” Wahab said.
“I was also told that people in Winnipeg are very nice and that it’s a great multicultural city which really appealed to me.”
Dr. Wahab completed his studies and ophthalmology residency from 2017 to 2021 at the University of Balamand in Lebanon. He also pursued his education and training at the American University of Beirut before moving to Toronto.
“I only lived in Toronto for one year; it’s a very big city,” Wahab said.
“While I liked it there, I knew it wasn’t for the long term.
“So, when the opportunity to come here came up, I knew it was the right timing. Plus, I really like seeing lots of green with the trees instead of tall buildings.”
Dr. Wahab said he loves the Wolseley area and adds the people at MHC have been very welcoming.
He said he would consider staying in Winnipeg once his fellowship year is complete.
“If there’s an opportunity to work at MHC I would need to discuss with my family and wife who is a physician and lives in Lebanon right now,” he said.
“But I would love to stay, we’ll see.”
When Dr. Wahab is not at work he loves to cook, read books and watch Formula 1 racing!
Easy Street supporting Manitobans on the long COVID front line
Easy Street supporting Manitobans on the long COVID front line

The worst of the pandemic may be over, but for many long COVID patients seeking care at MHC, the struggles seem endless.
Occupational therapist Tessa Bruce says 50 per cent of clients at Easy Street rehabilitation are now dealing with severe anxiety, brain fog, and fatigue.
“It is quite debilitating,” Bruce said. “From not being able to get dressed in the morning to not being able to shower.”
Bruce said treating long COVID patients is a complex and lengthy process.
“It is impacting their daily life activities like going outside for a walk, doing things they enjoy, or going to work.”
She said many of her clients are forced to take a leave of absence from work as they learn how to cope with their new reality.
“It’s very anxiety provoking because they lose their sense of identity,” Bruce said. “For many it’s a complete overhaul of your life.”
Easy Street, which specializes in cognitive rehabilitation, recently launched new six-week group sessions to help those on their long COVID journey, specifically those who are combatting brain fog and anxiety.
“I’m really excited about that because it offers peer support,” said Sarah Snider, another occupational therapist at Easy Street.
“I think there’s so much to be had in those learned experiences, so many people come to this program and say ‘wow, I never met anyone else with long COVID,’ so it’s all about that connection and shared experiences,” said Snider.
The concept of treating people with long COVID is also something that’s fairly new for practitioners at Easy Street which traditionally sees those with brain injury or stroke.
But Snider said there are a lot of parallels in the treatment for improving cognitive function.
The department recently held a long COVID event alongside experts from the University of Manitoba at the Manitoba Lung Association where they heard multiple stories from patients still living with long COVID symptoms. The event was for educational and research purposes.
Bruce said the whole team at Easy Street takes great pride in knowing they are helping so many people get their lives back.
“Everyone we see has different goals and milestones they want to reach, so this is very much a goal-based program, and the focus is all about our clients.”
A report from the Office of the Chief Science Advisor of Canada said that more than 1.4 million people in Canada, or about 15 per cent of adults who had contracted COVID-19 as of August 2022, say they experienced symptoms more than three months after being infected.
Meet Eye Care Centre of Excellence’s two new residents
Meet Eye Care Centre of Excellence’s two new residents

The eyes have always been fascinating organs for Dr. Katia Milovanova.
“There are a lot of beautiful things about ophthalmology,” she said. “I think the science behind how we see is very captivating, and the technology that we have now is just exhilarating.”
Milovanova is one of two new residents in our ophthalmology program this year and is more than ready to get started.
She said she loves the profession because she believes the results from this type of care is almost immediate compared to other medical specialties.
“I love that there is immediate feedback for the work you do,” she said. “The return is almost immediate with things like cataract surgery, treating eye infections for people, and then when their vision clears up it’s so incredible to see that.”
Dr. Parsa Mehraban Far is our other ophthalmology resident who is also eager to join the team at MHC. He did most of his medical training at Queen’s University in Ontario.
“For me personally it’s a very visual field, there’s very few other areas in medicine where you can directly see the pathology,” he said.
He moved to Canada from Iran when he was just 14-years-old and said he always knew he wanted to be an ophthalmologist.
“It’s a very rewarding profession in that I can see exactly what’s wrong with a patient, and why they can’t see well.
In the majority of cases, you can actually treat it and fix that problem,” Dr. Mehraban Far said.
“It’s also rewarding in the sense that you work with a lot of elderly people, but also people from lower social economic status who are disproportionately affected by many chronic illnesses like diabetes, high blood pressure and other causes of ocular pathology.”
He also likes that it’s a great mix of medicine and surgery.
“In ophthalmology you also do surgeries, so the combination of being able to do both [medicine and surgery] is what drew me to the profession,” he said adding he’s also enjoying his new life in Winnipeg.
“I really enjoy being in the city here,” he said. “I love the zoo, I got a membership now so I go there a lot!”
As for Dr. Milovanova, she grew up in Calgary and did most of her medical training in Edmonton. She moved to Winnipeg less than a year ago and she’s thrilled to be part of the Misericordia family.
“The people are lovely here, it almost has a grassroots environment feel to it,” she said.
“It’s an excellent place to train, the people are wonderful, and I’m very excited.”
New Operating Room Assistants join surgical team
New Operating Room Assistants join surgical team

MHC is thrilled to welcome two new Operating Room Assistants (ORA’s) who will soon be assisting our surgical care team.
Tara Soares and Norm Gibbons are no strangers to the Misericordia family. Both are long-time employees who started working on site as health-care aides.
“I actually started at Misericordia as a housekeeper and then transitioned into a health-care aide,” said Gibbons.
He said after 15 years working as a health-care aide he was moved into a new role as an OR Supply Assistant where he was able to learn a new set of skills.
“As a health-care aide you’re pretty much maxed out what you can do and learn, so when another new opportunity came up, I applied and just went for it.
“So far it’s been very interesting,” he said.
To qualify, Soares and Gibbons had to have at least five years of experience working as health-care aides in the OR. They also had to complete a 12-week online course through Mohawk College in Ontario which included stringent onsite testing in Manitoba.
“Some of the classes were challenging,” said Soares. “We learned everything from human anatomy to surgical anatomy to microbiology.”
The two new positions are part of a larger provincial plan to add 70 new operating room assistants across Manitoba. The aim is to reduce waitlists for diagnostic and surgical procedures as mandated by the province’s Diagnostic and Surgical Recovery Task Force.
Responsibilities will range from decontaminating rooms and disinfecting surgery equipment, to transferring and preparing patients safely for surgery.
Soares said she has learned so much working closely with patients over the years and is very excited to take on this new role.
“I’m really happy to be starting this next adventure,” Soares said.
“I like that I will be able to assist more, be with patients inside the surgery room and be involved in the surgeries.
“I’m feeling great, and I’m ready.”
Surgery nurse learning how aromatherapy may help patients
Surgery nurse learning how aromatherapy may help patients

A registered nurse at Misericordia Health Centre is hoping to add a new skill to her repertoire that could help her surgery patients deal with stress.
Amanda Lackey who currently works in the surgery department has been taking an online course to become a Clinical Aromatherapy Health Professional. The course is done through Joyessence Aromatherapy Centre, based out of Ontario.
“I’m definitely learning a lot of interesting things,” Lackey said. “You learn about different essential oils and how to use them to treat things like anxiety, or even coughs and colds.”
She said she’s learning about 72 different essential oils and their therapeutic uses.
“It should definitely never replace medical care—always make sure you seek medical care when needed—but it can be used along with your current medical care to help improve symptoms. It really helps!”
She hopes to incorporate what she learns about aromatherapy to her nursing assessment skills one day, especially when it comes to helping patients deal with anxiety before surgery.
Lackey points out there has been studies that show how certain aromas like sweet orange can decrease cortisol levels in people.
“I find it so fascinating, learning the chemistry behind it all,” she said. “The science on how it can just calm you or energize you.”
Lackey said she has always been interested in natural remedies and how it can be a boost to self-care.
“Right now, it’s more of a hobby, but could there be an opportunity down the road to become part of a medical study or to help in other areas within the facility here? Sure.”
Lackey said the course will take two years to complete but she’s already applying what she has learned so far in her personal life.
“I use aromatherapy when I’m at work—at lunch I have little inhalers so it doesn’t bother anybody else. There’s just so many things that it can help with.”
Ambulatory Care team says their patients are part of their family
Ambulatory Care patients are part of the family

Whether it’s the smiles from staff when you walk into the waiting area or the personal cards from patients posted on the walls, it’s easy to see why the Ambulatory Care team at Misericordia Health Centre considers themselves a tight knit family.
“When I first worked here there were still nuns here, it was a long time ago,” said Brad Black, a registered nurse in Ambulatory Care.
“But this has always been my home.”
Black has been part of the Misericordia Health family for more than 20 years, working in various departments within the facility.
The Ambulatory Care clinics serve many patients from all walks of life – in the city and those who travel to the city from rural communities for care.
On Tuesdays and Thursdays, it offers diabetic foot clinics where patients are assessed for ulcers, Charcot foot fractures and other conditions that affect the foot related to diabetes. Orthopedic specialists are present in the clinic on Mondays and Wednesdays.
While there are similar services offered at other health facilities in Winnipeg, Black says many people choose to access care from MHC. He says it’s about a sense of community.
“We work together as a team, and most of our patients come in regularly, we know them well, so they become part of our family,” Black said.
“We’re smaller, it’s familiar, and everybody gets treated with respect.”
The Ambulatory Care clinics have gone through many changes over the years. While it may be less busy due to a reduction in some services like Urgent Care, staff say the clinic is still vital to the community.
“Part of our clinic’s role is treating diabetic wounds,” said David Carroll who is a long-time orthopedic technologist at the clinic. “It’s specialized care.
“We cast people for ulcers but also Charcot foot fractures which is quite serious as it can cause the bones in your foot to be displaced, so it’s a very important program here.”
Carroll says regular casting for ankle and wrists also occur. Knee and hip injections to deal with painful joints are common.
Rosa Turkula is the unit clerk who has been with the team for 33 years. She’s known as the “gatekeeper” by her staff, and is the first face patients see when they walk in the clinic.
“I set the tone and greet the patients, and just make them feel comfortable,” Turkula said.
“When they come in I already know who they are.”
Her desk is adorned with thank you cards, photos and sweet messages from former patients and their families, many of them children.
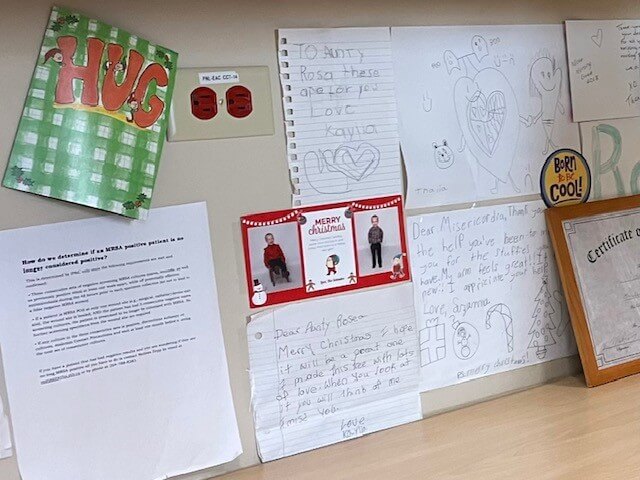
“I love all this,” she said. “It’s the little things like this you appreciate because you know they really love you here in the clinic.”
Turkula said many of the younger patients appreciate the stuffed teddy bears she offers them while they wait to receive care.
“This started many years ago when we were super busy doing casting care with younger patients at the time, some as young as three years old,” she said.
While the clinic doesn’t often do casting services for kids today, she said she continues to offer stuffed animals to any child waiting for care at Misericordia Health Centre.
Turkula says the small but mighty Ambulatory Care team makes it easy for her to come to work every day.
“We have our down days but other days make up for it,” she said.
“We all work together and help each other out, we care about our patients, it’s just a great place to work.”
Huddling for safety at MHC
Huddling for Safety at MHC
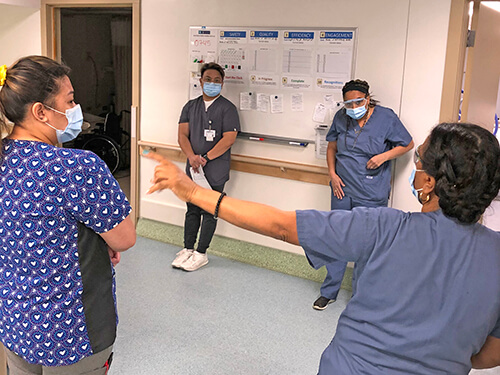
Karen McCormac, MHC’s director of quality and patient safety, may be getting a new nickname soon—coach.
Since last November Karen has been coaching MHC staff and managers on how to conduct Daily Safety Huddles. The huddles—essentially very short stand-up meetings—are billed by the WRHA as, “a proven way to improve safety and patient outcomes in health-care settings,” with well-documented benefits for health-care workers and the people they care for.
It takes up to three weeks for Karen to support managers to conduct daily huddles to advance staff and patient safety. The huddles will be taking place throughout MHC, including clinical and non-patient-facing areas. Each one takes a maximum of 15 minutes, though once comfortable with the process they are often over in as little as five minutes. Everyone is welcome—nurses, HCAs, unit clerks, patients, residents and families.
“The idea is to have an open dialogue about safety concerns—patient or staff related,” says Karen.
“The more we can talk and discuss issues in a safe, open way that gives people a chance to collaborate and contribute to solutions, the better outcomes we will experience for everyone.”
Huddles use a “Huddle Board” divided into quadrants to help focus responses on four areas—safety, quality, efficiency and engagement. The gatherings are a chance to identify ways to improve patient care, as well as to flag safety concerns that may relate to individual patients (e.g., if a patient is prone to falling the team can talk about their care plan) or all patients through universal process changes.
A ticket is created for any identified issues that need a solution. Tickets may be resolved immediately (e.g., a visit from plant services to fix a leaky sink) or may need to be escalated further up the huddle chain to an MHC leadership, regional or provincial huddle.
Time is also put aside for recognition of positive efforts, and everyone also gets a safety check-in.
“We go around the circle, make eye contact with each individual person, and ask ‘do you feel safe today? Is there anything you want to bring up?’”
The standardized Daily Safety Huddles are being rolled out at all WRHA sites.
#MHCFamily
COVID-19 treatment comes to Misericordia
COVID-19 treatment arrives at Misericordia
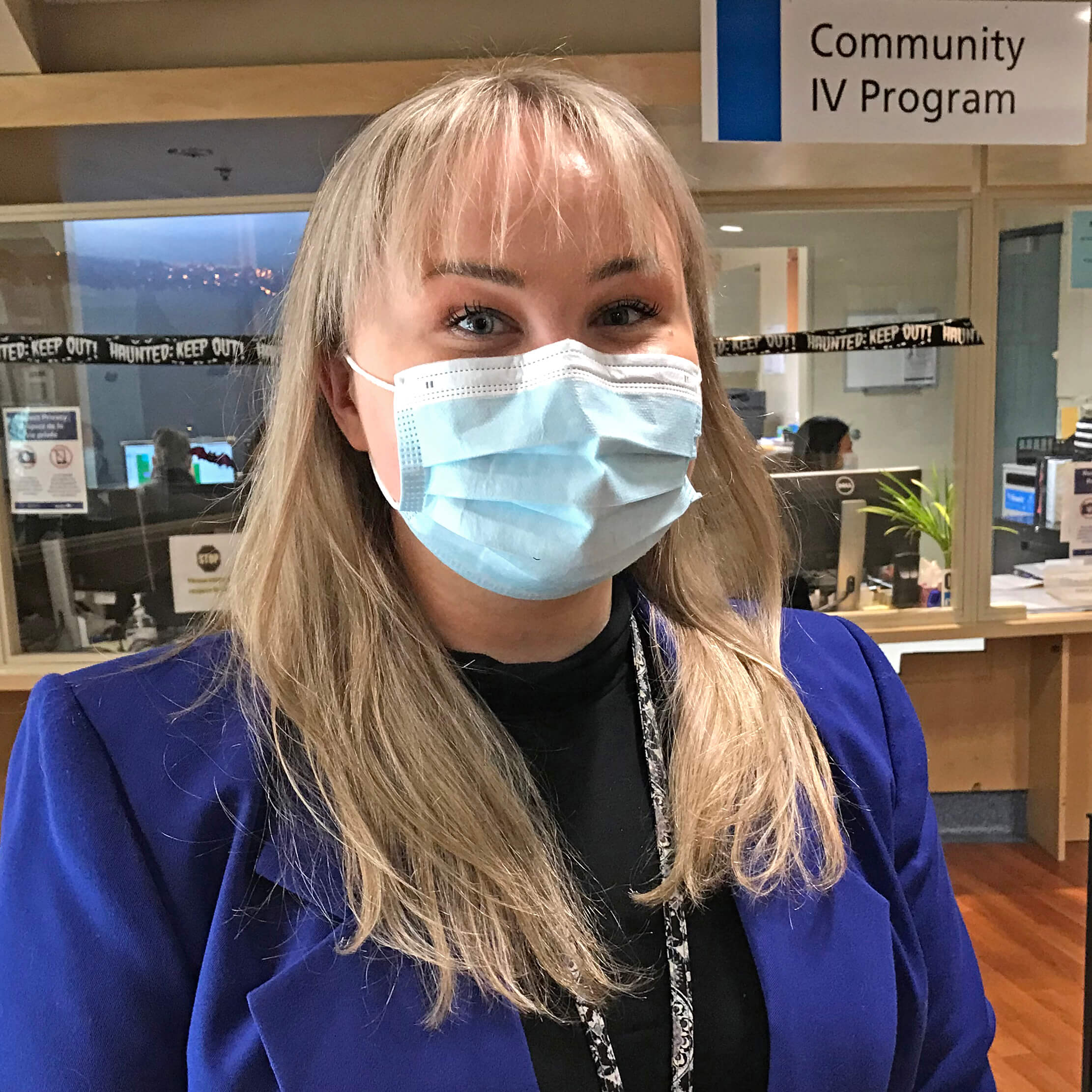
The Community IV Program (CIVP) team at Misericordia is helping create better outcomes for COVID-19 patients.
In August, CIVP began administering antiviral treatments to COVID-19-positive patients—treatments that had been previously performed at the Access Winnipeg West Primary Care Clinic.
“It was challenging at first,” says team manager Anna Mazur.
“Delivering the antiviral treatment is a very new process and an additional workload for everyone on our team—but we’re doing well.”
CIVP arrived at Misericordia in 2017 to treat various diseases with intravenous antibiotics. The multi-disciplinary team includes infectious disease physicians, nurses and pharmacists delivering medicine and providing wound care. They treat about 120 patients on site and in the community each day, seven days a week. Mazur says her team includes 75 nurses, along with administration staff to keep the program running smoothly.
The new Remdesivir antiviral treatments are being given to about six COVID-19-positive patients daily in a dedicated room at the CIVP site and in personal care homes. Patients must be referred by a doctor and meet eligibility criteria, which can include being immunocompromised or unvaccinated.
COVID-19 treatments have been delivered safely, Mazur says, thanks to approved operating procedures and infection control to protect patients and staff. She also credits her staff, which has worked hard and “showed a lot of strength and agility.”
#COVID19 #ProtectMB

